Introduction
The gut is a vital component of the human body and is one of the most complex portions of the body. It is often referred to as the second brain because of the correlations it has with other body parts. Systems like the gut-brain axis, the gut microbiome, and the digestive tract are all contained within the gut and regulate common bodily functions. Most importantly, the gut microbiome is home to a large number of microbial colonies that are responsible for keeping one healthy and in peak performance. Health of the microbiome is determined by the microbes themselves which reside in the gut. High quantities and diverse colonies are often what marks a microbiome as being healthy which is partially the reason why doctors and health enthusiasts promote the consumption of diverse foods mainly in the dairy and vegetable sections. Foods such as yogurt which promote microbial development are known as prebiotics. For most people, this would be the ideal way to promote a healthy microbiome within the gut, however, there are instances in which a substitute needs to be implemented. Probiotics are the substitute and can be a tool that could be instituted by both those who have an established prebiotic intake and those who do not. Probiotics can be in a multitude of different forms with the vast majority being powder or pills. They have the purpose of transporting large quantities of a variety of microbes straight into your gut with the hope of microbial reproduction in the microbiome. In recent years, discussions over the need for probiotic use in individuals have been heavily debated with sides supporting the use of probiotics and the side that probiotics are suboptimal in supporting microbiome health. After researching both sides of the argument, I have the position that probiotics are a beneficial and optimal tool for keeping the gut microbiome healthy.

Figure 1-Image of the intestinal track (5).
Popular Discussions and Viewpoints-
Whether or not probiotics are needed or beneficial has been discussed through recent studies in the scientific community. Those not in favor of using probiotics mainly have concerns with the digestive reactions, harm associated when regular drugs are used alongside probiotics, and the financial costs to institute regular supplements into your diet. Some studies have shown that certain probiotics have been linked to bloating and multiple other digestive issues. In addition to digestive responses, prescription drugs and pharmaceuticals for those requiring necessary medication have lost some of their effectiveness due to microbes found in probiotics. Mainly the financial burden of adding another “subscription” is disengaging people from using probiotics. Counter studies have been made, however, advocating for the use of probiotics in both individuals lacking healthy microbiomes as well as those with weakened microbiomes. These include the reliability of regulating the metabolism and digestive track, heightened immune response, and the counter to rising diary sensitivities and allergies. While I respect the merit of potential hazards associated with probiotics, higher quantities of beneficial impacts have been recorded, advocating for the use of probiotics.
Negative Digestive Responses from Probiotic Use
Steady metabolism and regular digestion are usually the signal indicating the health of one’s gut. Hindering either of them has vital impacts on both the weight and stool of an individual. Instances of probiotic usage altering both metabolism and digestion have been recorded through the Cleveland Clinic (2023). Instances of bloating and abnormal gas production in the stomach have been recorded. Bloating and abnormal gas production are drawbacks usually seen within the first few days or weeks of using probiotics. Usual occurrences of bloating have often come with discomfort and pain when trying to dispel the extra gas within the stomach. Mainly, reduced sleep and appetite have been linked to affects from bloating. Sleeping is already hard enough for some people and the additional discomfort from bloating is a serious issue when sleep is being deprived. In addition, bloating usually causes the loss of appetite due to the feelings of nausea and fullness. Loss of appetite can be harmful for those recovering from weight related eating disorders in which lower calorie intake was often the case. While these issues are usually observed for a brief time period after the first utilization of probiotics, they are still seen as a deterrent for people contemplating the use of probiotics.
Beneficial Impacts Associated with Digestion-
Probiotics have the main function of attempting to improve gut health and gut digestion. Multiple researchers have been studying the specific benefits relating to the microbiome on top of those relating to digestion. A study by Hemarajata and Versalovis (2012) outlined the direct correlation between probiotic mechanisms and how they manipulate multiple microbial colonies for beneficial purposes. Their study highlighted the possibility of improving intestinal barriers alongside reducing inflamed regions along the digestive track. The improved intestinal barriers are beneficial for reducing discomfort felt with stomach acid and gastroesophageal reflux. People who experience gastroesophageal reflux often would benefit from improved and repaired intestinal barriers. Similar studies were seen from Wilkins and Sequoia (2017) in which they highlighted that for optimal benefits, probiotic dosages should contain above 5 billion colony forming units per day. Anything less than 5 billion was observed to be inefficient for microbial growth. Information regarding reducing inflamed portions of the intestinal track were observed by both parties allowing for the notion that specific probiotics have the ability to prevent or reduce inflammatory conditions within the gut. Alongside inflammatory responses, stool samples were noted by the parties. Reduced instances of acute diarrhea and abnormal stool samples were observed to be correlated with the usage of probiotics. Practically those taking antibiotics were noted to have heightened chances of abnormal stool samples which was able to be prevented through the use of probiotics. Outlined notations from both parties showed improvements probiotics had on digestion and the digestive tract.

Figure 2-Mastication and the start of the digestive tract.
Effects Probiotics Have on Gastrointestinal Conditions
Gastrointestinal conditions are heavily linked to the microbiome of the individual associated. While some issues may be related due to precursory issues, for the most part the microbiome decides most of the gastrointestinal conditions experienced. Wilkins and Sequoia (2017) studied the effects probiotics had on specific conditions experienced in the gastrointestinal region. The most common microbes contained within the probiotics studied were Lactobacillus, Bifidobacterium, and Saccharomyces. While other microbes were observed, these were the most common strands associated in the study. The microbes mentioned showed significant benefits in mitigating or relieving a multitude of conditions including necrotizing enterocolitis, acute infectious diarrhea, ulcerative colitis, and multiple other conditions. Symptoms from these conditions were either completely reduced or mitigated to a point that is much easier to manage by the affected individual. However, there were some instances of failures exhibited in the study. Depending on which probiotic was used and the cause for gastrointestinal conditions, probiotics were shown to be ineffective at reducing symptoms. For example, acute infectious diarrhea caused by viruses seemed to have inconsistent results when probiotics were instituted, while causes from bacteria had significant improvements through the use of bacteria. This is expected because typical diseases have different medications associated with them. For example, viruses have vaccines and bacterial diseases have antibiotics. Crohn’s disease has been shown to be somewhat controversial. Certain symptoms from the disease were shown to be mitigated but the overall disease was either barely affected or not affected at all by the usage of probiotics. Similar to the study from Wilkins and Sequoia, a study was done over the use of probiotics for Inflammatory Bowel Disease (Ma et al, 2024). Fifty-three probiotics were used in the study which was aimed to determine the effectiveness probiotics had on reducing symptoms from inflammatory bowel disease. Probiotics were observed to regulate intestinal flora balance and repair the intestinal barriers of individuals. In addition, Bifidobacterium showed positive results in reducing the effects of inflammatory bowel disease. It can be determined that specific symptoms could be handled through the use of specific microbes. Mainly, specific conditions and causes require specific microbes to relieve symptoms or relieve the condition in total.
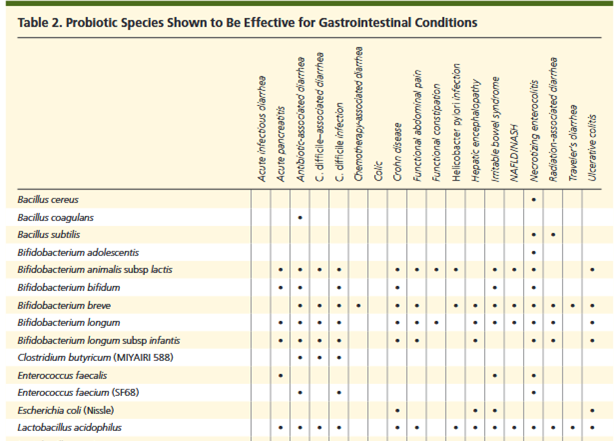
Figure 3- Table of gastrointestinal conditions that have been shown to be improved through the use of probiotics (16).
Gut-Brain Axis
Most people are unaware about the connection the gut and brain have between one another. Healthy guts are often seen to have strong connections along the gut-brain axis which is the connection between the intestinal tract and both the central and enteric nervous system. It promotes alertness, hormone regulation, and often controls aspects of mental health. Healthy microbial life in the gut has been linked to promoting alertness through neurotransmitters which is often why pro athletes take diet very seriously. Certain bacteria promote endogenous chemicals allowing for the communication between neurons. Probiotics have the capability of targeting the specific bacteria that help with this function. Furthermore, hormone regulation often occurred through the reactions between the gut and the brain. The gut microbiome is responsible for producing gut hormones from Enteroendocrine cells which act as signals for the gut brain axis. The hormones are then processed by the brain resulting in communication between both the gut and the brain. Sun, Li, Nie (2020) studied the relationship between the two and saw similar results. They concluded “gut hormones also play pleiotropic and important roles in maintaining health, and are key signals involved in gut-brain axis”. Hormone communication facilitates mental health and mental reactions. Oftentimes people with weaker gut health experience larger fluctuations in mood and personality. The opposite can be said for those with healthier guts. Those with healthier guts often experience more controlled mental reactions and stable personalities. Probiotics could be beneficial for regulating the connection in the gut-brain axis, mainly due to the regulation of the gut microbiota. As stated previously, the connection between the gut and brain is mainly affected by the microbes within the gut and how they stimulate communication. With that being said, probiotics facilitate microbial growth which leads to possible communication between produced hormones and the brain.
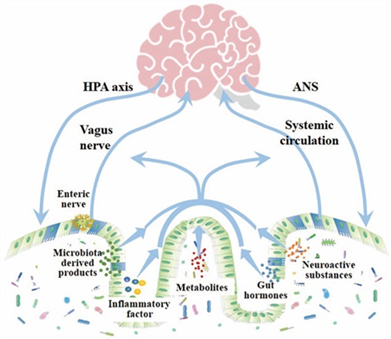
Figure 4-Relationship of the gut brain axis (12).
Probiotics Affecting Fiber Consumption
As stated previously, microbes have specific roles and functions inside the gut allowing for a multitude of various reactions. Various nutrient groups affect and are affected by microbes differently. Fiber is known to be one of the harder food groups to break down and digest for most of the population. Through the use of regular probiotics, microbes are able to effectively assist in the breakdown of these complex foods. Affective breakdown and digestion of fiber is vital in reducing potential risks of type 2 diabetes and heart diseases (Hicks, 2025). Furthermore, aiding the breakdown of fiber aids to the microbiome itself. Heightened fiber breakdown allows for quicker microbial transportation from food to gut, aiding in diversifying and replenishing the gut’s microbiome.

Figure 5- High fiber content foods based on daily suggestions.
Probiotics Affecting Protein consumption
Probiotics act as facilitators for protein absorption in the body. Probiotics are able to establish enzymes which increase the efficiency of protein absorption. More efficient protein consumption allows for quicker cell and tissue repairs throughout the body. Increased efficiency of protein absorption also aids in the transportation of amino acids and availability of protein synthesis in the body. Amino acid transportation aids in hormone responses and metabolic functions. Early on in life, the abundance of amino acids and the transportation of them have direct correlation to stimulating growth hormones in the body, in addition to controlling mood swings. Protein synthesis goes hand and hand with the production and transportation of amino acids. The more efficient production and transportation of amino acids allow cells the ability to create more proteins though protein synthesis (Trommelen et al, 2023). Probiotics directly affect the efficiency of multiple protein functions through the rapid digestion and absorption of proteins from enzymes.
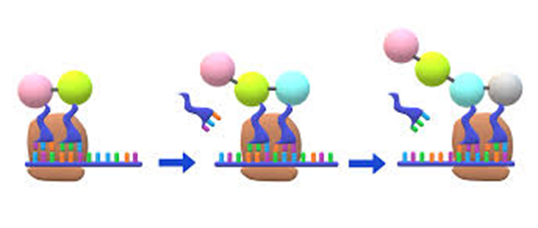
Figure 6-Simple cartoon of protein synthesis.
Probiotics Affecting Fat Consumption
Fats are often seen as the most controversial food group consumed due to their caloric density and relations to heart disease and type two diabetes. However, probiotics have been studied to show increased absorption and repurposing of fats within the intestines. Hicks (2025) reported how probiotics affect fats. She mentions how Lactobacillus rhamnosus GG has been shown to efficiently absorb fats in the intestines, which directly lowers the amount of fat absorbed by the actual body. Furthermore, Hicks reports that probiotics aid in modulating lipid and bile acid metabolism. Modulating lipid and bile acid metabolism aids in the utilization of fats and cholesterol which is often the concern that many have with consuming fats. Alongside aiding in absorption, probiotics promote the production of SCFAs or short chain fatty acids which have been linked to reducing inflammatory responses in the gut as well as promoting a stronger gut barrier. SCFAs have been linked to reducing potential cancers and boosting the immune system similar to certain microbes contained in probiotics. SCFAs are usually nominated as the healthy fats, however this correlation could be considered for an increased set of foods when probiotics are administered.
Probiotic Relations with Regular Drugs and Medications
Probiotics have the main function of reinstating microbes into an individual’s microbiome as stated previously. This function has the ability to interrupt specific needs an individual has with their specific medication. Depending on what microbes are present in the probiotic, they could target and lower the effectiveness of medications when taken. Data has been collected showing the relationship some probiotics have when drugs are administered. Microbes contained within probiotics have the ability to induce b-glucuronidases which is an enzyme designed to deconjugate xenobiotics. Deconjugation has been reported to lead to the formation of carcinogenicity which implies the formation of cancer, mainly in the colon (Merenstein et al., 2022). Aside from altering the effects of medications, microbes have the ability to dampen or fully mitigate the function of specific drugs. Probiotics have the ability to weaken the absorption of a medication resulting in an insufficient application of medicine. However, this is seen in very specific medication and probiotic reactions, which devalues the significance it has on whether probiotics should be instituted. There is additional information in the data collected in the same study that suggest probiotics have the ability to enhance the result medications have in their intended purpose. Furthermore, more research is being developed to conduct enzyme modifying medications, allowing for the intended purpose of the drug to work without worrying about the potential side effects from enzymes created from microbial contents in probiotics.

Figure 7-Simple image of medication.
Probiotics Affecting the Metabolic Profile of the Urinary System
Other metabolic profiles and their reactions to probiotics are being examined alongside the gut’s reaction. The urinary system is one of the profiles being examined in response to probiotics. Studies show that probiotics have the ability to alter metabolites in both the urinary and serum system, without altering the entire metabolic profile of the individual. Microbes transported from probiotics to the gut microbiome showed signs of creating similar urinary patterns between those taking probiotics (Cesare et al., 2023). Administered probiotics were able to ridden the difference of urinary and serum metabolic profiles of individuals taking probiotics. Eliminating the difference or uncertainty of metabolic profiles allows for better tracking and examinations of the human body in regards to potential treatments for urinary diseases or conditions.
Potential Toxins Found in Probiotics
Side effects are nearly always present when supplements are involved. With that being said, certain probiotics have been found to occasionally produce episodes of toxicity within the gut. Reports from Doron and Snydman (2015) showed that different populations experienced varying levels of toxicity. Data from Pop, Suharoshi, and Gabbianelli (2022) suggest that common probiotics have the ability to promote carcinogen absorption within the body, promoting cancers within the gut. Carcinogens are usually consumed with the potential risk of exposing your body to danger. Probiotics are no different. There is the possibility that very specific microbes can unleash toxins promoting negative affect. However, alongside the potential harm, the same studies provided information that probiotics have the capability of lowering toxicity within the gut or altering their composition. Lactobacillus has the ability to bio detoxify substances which causes probiotics to be relatively safe for consumption.
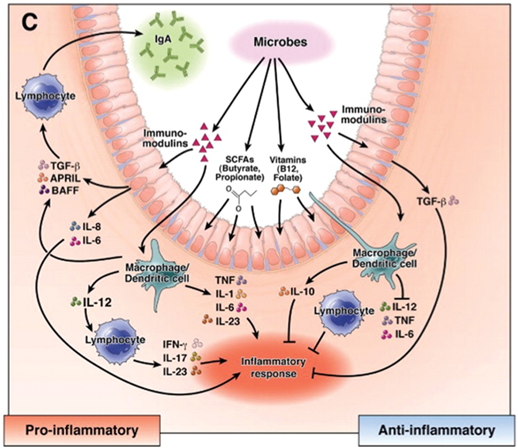
Figure 8-Probiotics affecting the immune system with the creation of SCFAs, aiding in anti-inflammatory responses along the intestinal tract (6).
Strengthen Immune Response
Microbial activity has the potential to stimulate immune response to bacterial diseases. Instituting probiotics in one’s daily routine has the capability of alleviating the need for antibiotics in health systems. Bacterial diseases like food poisoning are often relieved through the use of antibiotics which has both beneficial and harmful effects. Antibiotics are known to kill both harmful bacteria in the gut as well as the beneficial ones, weakening the gut microbiome. This change can lead to the potential reoccurrence of bacterial diseases. Altering the reliance of antibiotics and using probiotics as a substitute could mitigate both the possibility of contracting bacterial diseases along with the side effects associated with the disease. Probiotics have the fundamental purpose of adding additional microbes in the gut, which is usually the issue that many people have when contracting food poisoning. Individuals who travel to outside countries such as Bali, usually experience food poisoning very quickly. This is because foods and liquids consumed in the foreign countries are new to the body. They contain microorganisms that are usually absent in regular diets and are introduced through travel. Probiotics would limit the possibility of experiencing bacterial diseases through prior contact of individual bacteria. Similar to the function vaccines have with making the body experience a limited amount of a virus before contracting the virus, probiotics would be doing the same thing. For instances such as E-coli, probiotics would be able to limit the possibility of experiencing negative side effects.
Rise of Dairy Sensitivities
Dairy products have been an established food group in multiple cultures for a multitude of years. As time has progressed, the reliance of dairy-based foods has altered which is causing a rise of dairy sensitivities and allergies. A survey created by Warren (2022) included responses from 79,000 individuals in the US showed that around 7.5% of people had some sort of sensitivity or allergy to milk products. Females are at a greater risk of containing these sensitivities alongside specific demographics in the population. Ages ranging from 1-3 and 18 on were seen to exhibit larger quantities of milk related sensitivities. Thinking about personal experiences, there’s a good chance you know multiple people who have said they experience some sort of sensitivity or allergy to dairy. This may be a result of increasing population or it could be a sign that dairy sensitivities are on the rise.
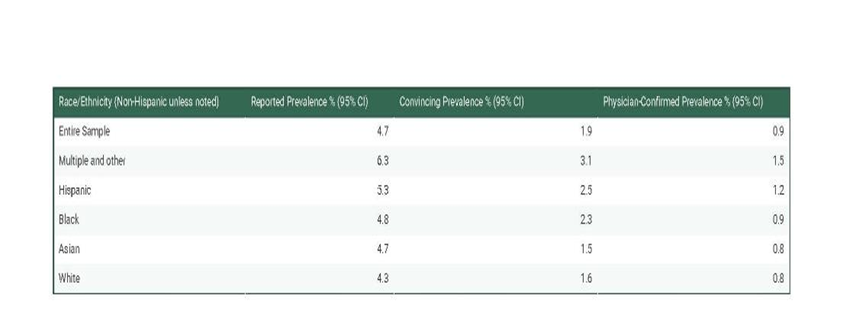
Figure 9-Percentages of Cow milk allergens by race in the us (14).
How do Dairy Sensitivities Affect the Microbiome?
Most people aware of the microbiome utilize yogurt and other fermented dairy products as their main source of prebiotics. However, with the increased sensitivity to dairy related products as shown by Warren (2022), more people are hindered on their ability to consume dairy related prebiotics. There is the alternative of plant-based prebiotics, however, there is a case for the same discussion involving allergies. Allergies are prevalent for everyone and for each person allergic to dairy, there is a good chance that a similar fraction of the population experiences allergic reactions to plant-based prebiotics. Hindrances like dairy sensitivity often cause people to have lower populations and diversity of microbes within their gut, lowering the overall health of their microbiome. Often time, immune response, regulated digestion, and alertness are all hindered as a result of less healthy microbiomes. This is when substituting to probiotics would become a helpful tool for individuals experiencing hindrances in their prebiotic use. Alleviating the reliance of prebiotics would grant everyone the capability of establishing their microbiome without any of the side effects from sensitivities and allergies.
Concluding Information
While side effects have been witnessed through the administration of probiotics, they are relatively uncommon and are outweighed drastically by the benefits. With that being said there is merit to the negatives. Possible toxic formations, lowered effectiveness of issued drugs, and the financial costs of regular usage of probiotics are all potential deterrents for the use of probiotics. Even so, benefits to digestion, nutrient absorption and utilization, accessibility, immune response, and stronger connections in the gut-brain axis show massive upsides with the implementation of probiotics. They are able to reliably regulate the gut and intestinal pathway through microbial functions found in the microbiome. Different microbes allow for the ease of nutrient absorption and utilization such as fats and proteins. Stimulating the presence of short chain fatty acids and processes such as protein synthesis. Nutrient utilization is important for a multitude of functions such as rebuilding cells and rebuilding intestinal barriers.
Additionally, probiotics are accessible to all parts of the population which cannot be said for prebiotics. Prebiotic sensitivities and allergies allow only a percentage of the population to benefit while probiotics can be offered to all. This permits those with dairy sensitivities the ability to strengthen their microbiome without harming themselves.
Probiotics heighten the immune system and could possibly become the new antibiotic in some cases. Bacterial diseases could potentially be relieved or mitigated through the administration of probiotics before the disease becomes prevalent. When usage is done regularly, bacterial diseases have been shown to lower in abundance along with mitigating the harmful effects. Ultimately, probiotics have a huge upside in relation to both gut health and overall health. A healthy gut means a healthy life for most people. This is often overlooked which gives reasoning for the establishment of probiotics in one’s daily life.
Bibliography
- Can You Make Your Gut Healthier with Probiotics? (2023, July 21). ColumbiaDoctors. https://www.columbiadoctors.org/news/can-you-make-your-gut-healthier-probiotics
- Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology : Quarterly Publication of the Hellenic Society of Gastroenterology, 28(2), 203–209.
- Di Cesare, F., Calgaro, M., Ghini, V., Squarzanti, D. F., De Prisco, A., Visciglia, A., Zanetta, P., Rolla, R., Savoia, P., Amoruso, A., Azzimonti, B., Vitulo, N., Tenori, L., Luchinat, C., & Pane, M. (2023). Exploring the Effects of Probiotic Treatment on Urinary and Serum Metabolic Profiles in Healthy Individuals. Journal of Proteome Research, 22(12), 3866–3878. https://doi.org/10.1021/acs.jproteome.3c00548
- Doron, S., & Snydman, D. R. (2015). Risk and Safety of Probiotics. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 60(Suppl 2), S129–S134. https://doi.org/10.1093/cid/civ085
- Gut check: What UAB experts say about probiotics, digestion, and your microbiome – Heersink School of Medicine News. (n.d.). Retrieved September 18, 2025, from https://www.uab.edu/medicine/news/microbiology/gut-check-what-uab-experts-say-about-probiotics-digestion-and-your-microbiome
- Hemarajata, P., & Versalovic, J. (2013). Effects of probiotics on gut microbiota: Mechanisms of intestinal immunomodulation and neuromodulation. Therapeutic Advances in Gastroenterology, 6(1), 39–51. https://doi.org/10.1177/1756283X12459294
- Kluijfhout, S., Trieu, T.-V., & Vandenplas, Y. (2020). Efficacy of the Probiotic Probiotical Confirmed in Acute Gastroenteritis. Pediatric Gastroenterology, Hepatology & Nutrition, 23(5), 464–471. https://doi.org/10.5223/pghn.2020.23.5.464
- Ma, Y., Yang, D., Huang, J., Liu, K., Liu, H., Wu, H., & Bao, C. (2024). Probiotics for inflammatory bowel disease: Is there sufficient evidence? Open Life Sciences, 19(1), 20220821. https://doi.org/10.1515/biol-2022-0821
- Mazziotta, C., Tognon, M., Martini, F., Torreggiani, E., & Rotondo, J. C. (2023). Probiotics Mechanism of Action on Immune Cells and Beneficial Effects on Human Health. Cells, 12(1), 184. https://doi.org/10.3390/cells12010184
- Merenstein, D., Pot, B., Leyer, G., Ouwehand, A. C., Preidis, G. A., Elkins, C. A., Hill, C., Lewis, Z. T., Shane, A. L., Zmora, N., Petrova, M. I., Collado, M. C., Morelli, L., Montoya, G. A., Szajewska, H., Tancredi, D. J., & Sanders, M. E. (n.d.). Emerging issues in probiotic safety: 2023 perspectives. Gut Microbes, 15(1), 2185034. https://doi.org/10.1080/19490976.2023.2185034
- Pop, O. L., Suharoschi, R., & Gabbianelli, R. (2022). Biodetoxification and Protective Properties of Probiotics. Microorganisms, 10(7), 1278. https://doi.org/10.3390/microorganisms10071278
- Sun, L.-J., Li, J.-N., & Nie, Y.-Z. (2020). Gut hormones in microbiota-gut-brain cross-talk. Chinese Medical Journal, 133(7), 826–833. https://doi.org/10.1097/CM9.0000000000000706
- Trommelen, J., van Lieshout, G. A. A., Nyakayiru, J., Holwerda, A. M., Smeets, J. S. J., Hendriks, F. K., van Kranenburg, J. M. X., Zorenc, A. H., Senden, J. M., Goessens, J. P. B., Gijsen, A. P., & van Loon, L. J. C. (2023). The anabolic response to protein ingestion during recovery from exercise has no upper limit in magnitude and duration in vivo in humans. Cell Reports Medicine, 4(12), 101324. https://doi.org/10.1016/j.xcrm.2023.101324
- Warren, C. M., Agrawal, A., Gandhi, D., & Gupta, R. S. (2022). The US population-level burden of cow’s milk allergy. The World Allergy Organization Journal, 15(4), 100644. https://doi.org/10.1016/j.waojou.2022.100644
- What Are Probiotics & What Do They Do? (n.d.). Cleveland Clinic. Retrieved October 30, 2025, from https://my.clevelandclinic.org/health/treatments/14598-probiotics
- Wilkins, T., & Sequoia, J. (2017). Probiotics for Gastrointestinal Conditions: A Summary of the Evidence. American Family Physician, 96(3), 170–178.
- Xiong, R.-G., Zhou, D.-D., Wu, S.-X., Huang, S.-Y., Saimaiti, A., Yang, Z.-J., Shang, A., Zhao, C.-N., Gan, R.-Y., & Li, H.-B. (2022). Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods, 11(18), 2863. https://doi.org/10.3390/foods11182863